Menstrual cycle and period: Phases, hormonal influences, tracking tips, and menstrual issues
Menstruation is a normal occurrence in women of reproductive age. Its length and pattern may vary from person to person. However, amidst the variations, science has set a range that determines normalcy. Read on to learn more about the menstrual cycle, how to calculate yours, and when to speak with a doctor about menstrual issues.
Written By
Queendaleen Okeke-izuagwuHealth writer⏐Nurse (RN)
Reviewed By
Azuka Chinweokwu EzeikeMedical Doctor (MBBS), MSc(PH) | Consultant Obstetrician & Gynecologist
Key takeaways:
- The menstrual cycle occurs in phases and is influenced by female reproductive hormones such as estrogen, progesterone, follicle-stimulating hormone, and luteinizing hormone.
- Several factors, such as stress, medications, or illnesses, can impact the length and pattern of the menstrual cycle.
- See a doctor, particularly a gynecologist, if you notice any unusual changes in your menstrual cycle or period, or if you're experiencing any of the menstrual problems mentioned in this article.
Each month, various physiological changes (in the form of the menstrual and ovarian cycles) occur in the female body to prepare the body for possible pregnancy.
Female hormones regulate these changes, and an imbalance in any of the hormones involved can impair these physiological occurrences. Aside from hormonal imbalance, other factors, such as stress, certain medical conditions, or medications, can influence the length and regularity of the menstrual cycle.
What is the menstrual cycle?
The menstrual cycle is a process people assigned female at birth experience to prepare the body for pregnancy. It involves a series of hormonal changes and physiological events that occur every month to prepare the body for pregnancy.
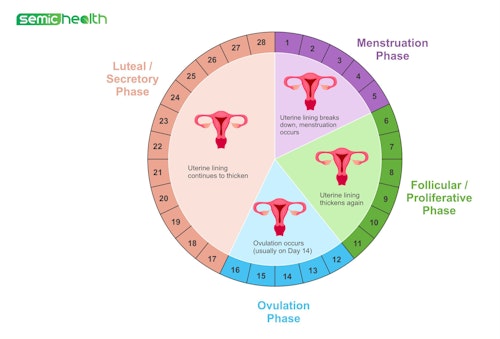
Each menstrual cycle consists of phases that begin on the first day of your period and end on the day before the next period begins. The average length of the menstrual cycle is about 28 days, although it varies from person to person between 21-35 days.
Period, also called menstruation or menstrual flow, is one of the menstrual cycle events. It involves the shedding of some layers of the uterus lining (endometrium). This typically comes out as blood.
The hormonal changes that occur throughout the cycle can lead to various physical and emotional changes in individuals. The events that make up the menstrual cycle can be divided into the uterine cycle (changes in the uterus) and the ovarian cycle (changes in the ovary), with each cycle occurring in phases.
Phases of the menstrual cycle and what happens in each phase
The phases of the menstrual cycle are marked by changes that occur in the uterus and ovaries at the same time.
The phases in the uterine cycle include:
1. Menstruation phase
The phase of menstruation, commonly called period, marks the beginning of the menstrual cycle and involves the shedding of some lining of the uterus and the passage of some amount of blood through your vagina.
Progesterone and estrogen levels are at their lowest in this phase. The menstruation phase lasts about 2–7 days in each menstrual cycle.
The most visible symptom of menstruation is the discharge of blood from the vagina, which results from the shedding of the uterine lining. However, most people experience several other symptoms during this period. Symptoms of menstruation can vary in intensity from person to person and cycle to cycle.
Other symptoms of menstruation may include abdominal cramps, bloating breast tenderness, headaches, fatigue, mood changes, and acne. While these symptoms are common, their severity and impact vary widely among individuals.
2. Proliferative phase
This phase begins immediately after menstruation and lasts until ovulation. It typically lasts from around the 5th to 14th day in a 28-day cycle, although individual variations can occur.
During the proliferative phase, the endometrium (which part of it is being shed out during menstruation) starts thickening in response to the increasing levels of estrogen. This occurs in preparation for the implantation of a fertilized egg (in case fertilization occurs).
Additionally, the cervical mucus becomes thin, clear, and slippery (having the texture of egg white), facilitating sperm movement and increasing the chances of fertilization.
The proliferative phase sets the stage for ovulation, which marks the transition to the next phase, the secretory phase.
3. Secretory phase
The secretory phase is the third phase of the menstrual cycle, following ovulation. In a 28-day cycle, the secretory phase lasts from around the 15th to the 28th day. This phase has a constant duration of 14 days.
During the secretory phase, progesterone levels rise, causing the uterine lining to become thicker and richer in blood supply, preparing the uterus for the potential implantation of a fertilized egg. Also, cervical mucus becomes thicker, making it less easy for sperm to pass into the uterus, thereby acting as a barrier to prevent further fertilization after ovulation.
Ovarian cycle phases that overlap with the menstrual cycle
The menstrual cycle occurs at the same time as the ovarian cycle, (characterized by events happening in the ovary). In the ovaries, the following phases occur:
Follicular phase
The follicular phase begins on the first day of menstruation and lasts till ovulation. It overlaps with the menstruation and proliferative phases of the uterine cycle. During this phase, follicle-stimulating hormone (FSH) is released by a part of the brain called the pituitary gland.
The FSH stimulates the growth of ovarian follicles, each containing an immature egg. As the follicles develop, one dominant follicle emerges and matures in preparation for ovulation.
The follicles also produce estrogen, which causes the endometrium to thicken, as in the proliferative phase. This phase lasts about 10-14 days.
Ovulation phase
Around the mid-cycle, usually around the 14th day in a 28-day cycle, the dominant follicle in one of the ovaries ruptures and releases a mature egg. This release results from a surge of luteinizing hormone (LH) and is called ovulation. The egg travels down the fallopian tube, where it can be fertilized by sperm (if good-quality sperms are present).
Usually, one egg is released during each cycle. However, in some cases, a woman may release two eggs in a cycle. The released egg is viable for fertilization for about 12–24 hours.
Luteal phase
After ovulation, the ruptured follicle transforms into a structure called the corpus luteum. This structure secretes progesterone and some estrogen, which help maintain the thickened endometrial lining, preparing it to receive a fertilized egg.
If fertilization does not occur, the hormone levels drop, leading to the shedding of the endometrial lining, resulting in menstruation.
The luteal phase occurs at the same time as the secretory phase of the uterine cycle and lasts about 12–14 days.
Female reproductive hormones involved in the menstrual cycle
The female reproductive system is influenced by hormones regulated by a part of the brain called the hypothalamus. The hypothalamus produces a hormone called the gonadotropin-releasing hormone (GnRH), which is the chief hormone that regulates the production of male and female sex hormones.
In males, GnRH influences the production of testosterone, while in females, it influences the production of estrogen and progesterone. GnRH causes the cells in the pituitary gland to produce FSH and LH. These two hormones travel down to the ovaries to influence the production of estrogen and progesterone. Here's an in-depth explanation of each hormone:
1. Follicle-stimulating hormone (FSH)
FSH is a hormone produced by the pituitary gland. Its primary role is to stimulate the growth and development of ovarian follicles during the follicular phase. FSH promotes the maturation of these follicles containing immature eggs. As the follicles grow and mature, they produce estrogen.
The increasing production of estrogen as the cycle progresses signals the pituitary gland to decrease the production of FSH while increasing the luteinizing hormone (LH).
2. Luteinizing Hormone (LH)
The pituitary gland secretes LH, just like FSH. LH functions mainly to trigger ovulation.
LH levels peak around mid-cycle. This surge stimulates the rupture of the dominant mature follicle and the release of an egg. After ovulation, the remaining follicle transforms into corpus luteum, which produces progesterone. At this time, the level of LH starts reducing alongside estrogen.
3. Estrogen
Estrogen is a hormone primarily produced by the growing ovarian follicles, especially the dominant follicle. It plays an important role throughout the cycle. Increasing estrogen levels in the follicular phase promotes the growth of the endometrium in preparation for implantation.
Estrogen also stimulates the production of slimy cervical mucus, which helps in the movement of sperm through the cervix and into the uterus. Also, high levels of estrogen, along with the LH surge, trigger ovulation.
After ovulation, estrogen levels temporarily decline but rise again later in the cycle to help maintain pregnancy if conception occurs.
4. Progesterone
The primary source of progesterone production is the corpus luteum, which is formed from the remnants of the ovarian follicle after ovulation. Its main role is to support pregnancy. It does this by maintaining the thickened endometrial lining for suitable implantation and inhibiting uterine contractions that could potentially lead to the dislodging of the implanted embryo.
If pregnancy does not occur, the corpus luteum degenerates and results in a decrease in progesterone production. This decline triggers the shedding of the endometrial lining, known as menstruation, and the menstrual cycle begins again.
These four hormones work together in a regulated feedback mechanism, ensuring the proper development and function of the reproductive system during the menstrual cycle.
Recommended:
How to calculate the menstrual cycle
Although the normal length of the cycle ranges between 21 and 35 days, it is important that you know how to calculate your menstrual cycle so you'll be aware of your fertile window (the days you are most likely to get pregnant).
To calculate your menstrual cycle and determine its length, these steps can be followed:
- Note the first day of your menstruation as day 1 of your cycle.
- Track the last day before your next menstruation starts. This marks the end of your cycle.
- Count the number of days from day 1 of your current cycle to the day before your next period begins. For example, if your period starts on 18th April and the next period starts 15th May, your cycle length is 27 days because your current cycle ended on the 14th May.
- Do this for a few months to determine if your cycle is regular or not.
- If it is regular, then you have your cycle length.
- If not, the tracked cycles for the number of months will give you hints on the range of your cycle length.
- Also, to get the average length of your cycle, you add up the number of cycles tracked and divide by the number of months. For example, if your calculated six cycles are 26, 28, 30, 26, 25, and 27. To get your average cycle length: 26+28+30+26+25+27= 162. 162÷6 (months)= 27 days
Therefore, your average cycle length is 27 days.
By tracking your cycle over several months, you can get a better understanding of the length and pattern of your cycle. This can help track fertility or identify any irregularities.
Additionally, understanding when ovulation occurs is important. This may be more important for those trying to conceive or avoid pregnancy. The use of ovulation kits, tracking basal body temperature, and monitoring cervical mucus changes are some methods used to predict ovulation.
You're most likely to get pregnant 5 days before your ovulation to about 24 hours after your ovulation. This is because sperm can live up to 5 days in a woman's body, and your egg is viable for fertilization between 12-24 hours after ovulation. The fertile period may extend beyond this period, as the exact time of ovulation is unpredictable.
Things that can alter the menstrual cycle
Several factors can alter the length or pattern of the menstrual cycle. Some of these include:
1. Stress
Physical and emotional stress can affect the levels of the female reproductive hormones, resulting in irregular periods or even missed periods.
2. Dietary factors
Poor nutrition or extreme weight-loss diets can impact hormone production and cycle regularity.
3. Weight Changes
Significant weight gain or loss can disrupt the balance of hormones and affect the pattern of menstrual cycles.
4. Medications
Medications, such as hormonal contraceptives, antipsychotics, or chemotherapy drugs, may cause hormonal imbalances, leading to irregular menstrual cycles.
5. Medical Conditions
Conditions such as thyroid disorders, polycystic ovary syndrome (PCOS), hormonal imbalances, or other reproductive system issues that may cause fluctuations in hormone levels, including estrogen and progesterone, can influence the regularity of the menstrual cycle.
6. Perimenopause
As women approach menopause, hormone levels begin to fluctuate naturally, resulting in changes in the menstrual cycle.
It's important to note that it's normal to have occasional irregularities in your menstrual cycle due to some changes in the body. However, significant or persistent changes should be discussed with a healthcare provider, particularly a gynecologist.
Common menstrual problems
Some common menstrual problems include:
- Premenstrual syndrome (PMS): PMS refers to the physical and psychological symptoms that may occur a week or a few days before your menstruation. Some symptoms include abdominal cramping, breast heaviness and pain, mood swings, and heightened cravings. A severe form of PMS known as premenstrual dysphoric disorder (PMDD) may also occur, in which case you may need to see a doctor.
- Dysmenorrhea: This refers to painful cramps during menstruation.
- Menorrhagia: This means having heavy bleeding, including prolonged periods in a normal cycle length.
- Metrorrhagia: It means bleeding in between periods. Bleeding that is not the regular mid-cycle ovulation spotting may need medical attention.
- Oligomenorrhea: This refers to having infrequent periods.
- Amenorrhea: Amenorrhea simply means an absence of menstruation
When to speak with a doctor about menstrual issues
You need to see a doctor if you experience any of the following:
- Periods lasting less than 2 days or more than 7 days
- Heavy bleeding that soaks two or more pads or tampons each hour for two hours in a row
- Menstrual cycle less than 21 days or more than 35 days
- Severe premenstrual syndrome (PMS)
- Extreme period pain or discomfort that interferes with your activities
- Scanty menstruation
- Persistent or significant irregular cycles, if you have been having regular cycles
- Bleeding in between periods
- If you don't see your period for 3 months (90 days) and you're not pregnant or breastfeeding
Frequently Asked Questions (FAQs)
How long does a normal period last?
When in life do periods start and stop?
Is the 21-day menstrual cycle normal?
How much bleeding is normal during my period?